




Family Health
The Latest Trends and Recommendations for COVID-19, Influenza and RSV
Published: Jan. 4, 2024

If the holiday season left you with a pesky cough, runny nose or worse, you’re not alone. The number of COVID-19 cases and COVID-19-related hospitalizations – especially locally – are significantly ramping up and on par for this time last year.
What’s unique is the number of influenza and RSV cases we’re seeing already – significantly higher than last year. And it’s worth asking: What’s different between this year and last?
While the days of masking and other similar precautions seem like a distant memory, they’re really not all that far behind us. Last winter, many of us were still masking in and out of hospital settings and adjusting activities based on current spread. In 2023, most medical facilities lifted mask mandates, and many of us returned to the activities we had avoided or missed out on during the past couple years.
I think it’s a fair suspicion that a shift in our behaviors coupled with our usual travel, family gatherings and indoor activities this time of year has led to an increase of not only COVID-19 cases, but also the flu and RSV.
The Clear Front-Runner
In Nebraska and Iowa, COVID-19 cases significantly outpace influenza and RSV. The flu comes in second – with Influenza A being the current dominant strain – but RSV is not far behind this year.
The current COVID-19 variant causing the majority of infections across the country is JN.1. This is the Omicron variant that was first seen in the fall and has outcompeted the other strains over the last couple months. It remains very infectious – as all circulating variants have been – but there’s not enough evidence to suggest that it causes more severe disease than previous variants.
A Refresher on Vaccines
Everyone 6 months or older should consider the flu vaccine and updated COVID-19 booster.
The updated booster, which targets the current circulating COVID-19 strain, is effective in significantly decreasing your likelihood of developing severe disease and being hospitalized. Some more recent studies also suggest that the updated booster can generate immunity that may help decrease your likelihood of even contracting the disease for at least one to two months – a significant portion of the remaining respiratory virus season.
RSV is a virus that likes to primarily pick on infants and older adults. For this reason, the RSV vaccine is recommended for those over the age of 60. It’s also recommended for pregnant women in their third trimester, as antibodies generated by this vaccine are passed on to the otherwise vulnerable baby. We don’t have a vaccine for infants at this time, although there are antibody treatments that can be considered for infants who are at risk for RSV.
In short, it’s certainly not too late to get vaccinated, as we still have a lot of COVID-19, flu and RSV season left.
Testing and Appropriate Care
There seems to be a circulating misconception that if a person tests negative for COVID-19, they’re negative – period.
As we’ve learned, COVID-19 testing can be very dependent on timing. Unlike in flu cases – where you’re more than likely to get a positive test result in the first couple days of symptom onset – the vast majority of patients who test positive for COVID-19 will do so if testing occurs on the fifth day of symptom onset or later. This is because the COVID-19 virus continues to replicate in the first few days of infection, creating more genetic material and viral proteins that these tests are looking for. If you test negative in the first few days of symptom onset, it’s reasonable to test again in another couple days.
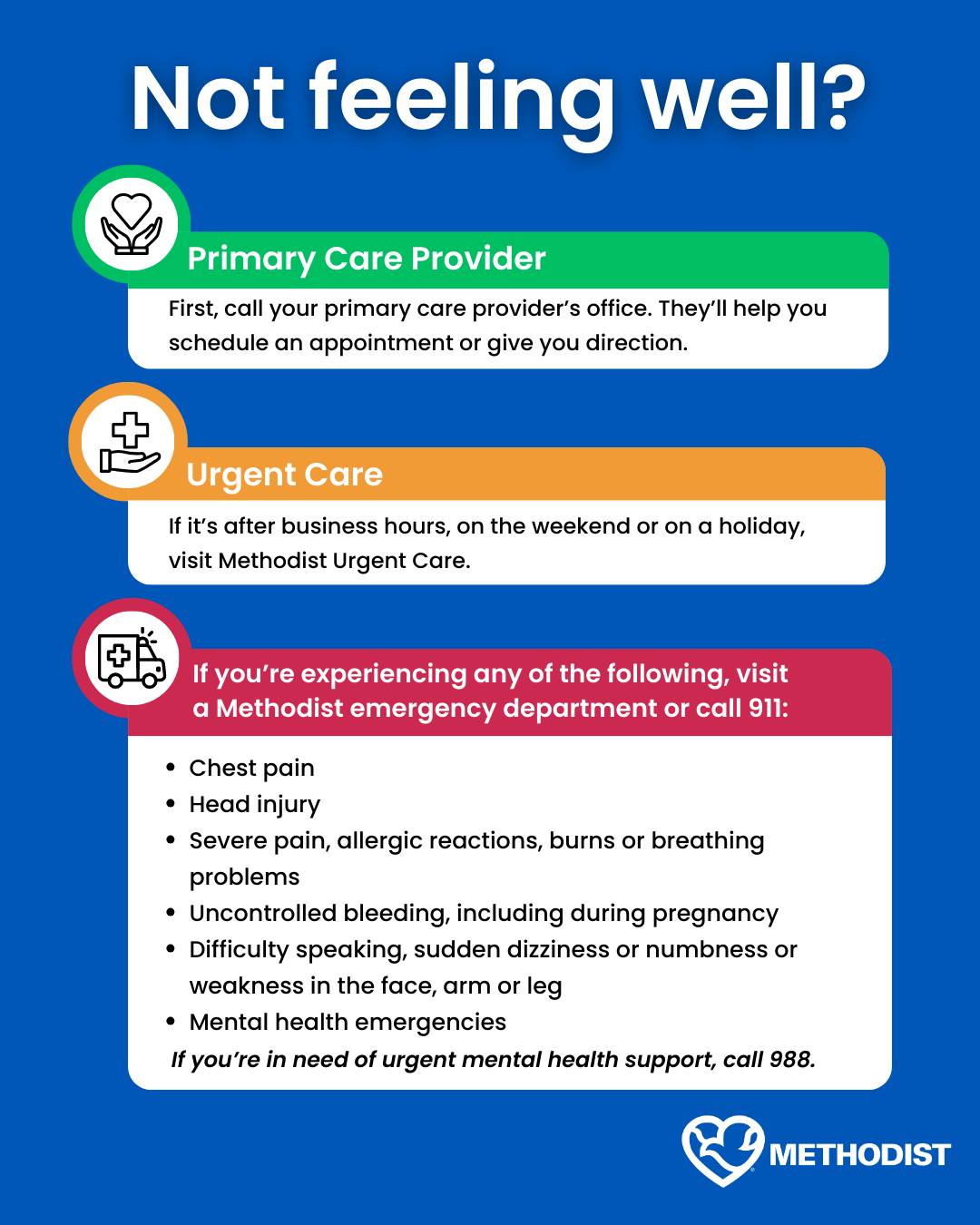
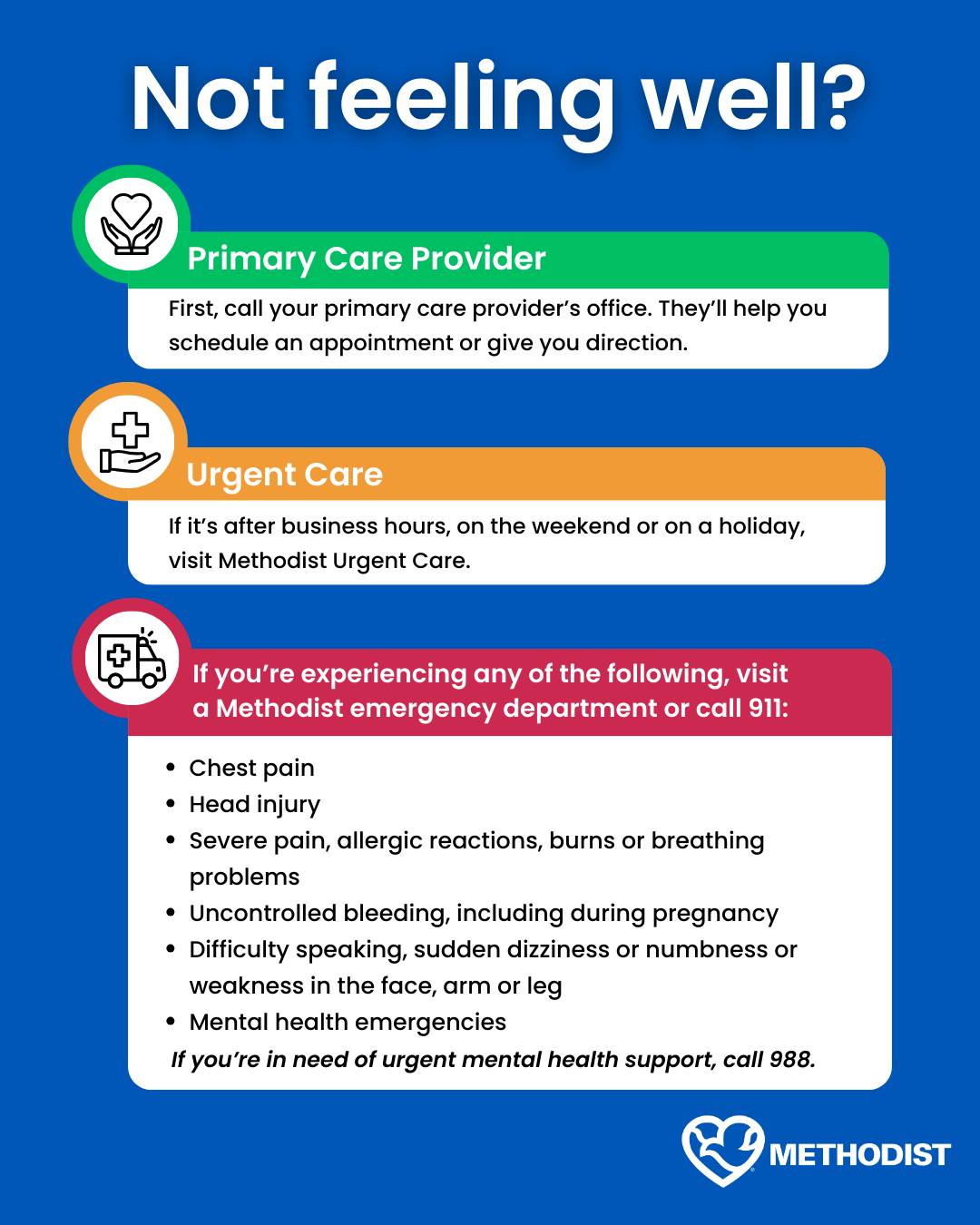
It's important to note that clinical and at-home COVID-19 tests are both quite effective. So, you really don’t need to be tested in a clinic or the emergency department (ED). Lately, Methodist EDs have been inundated with COVID-19-related cases, which warrants a reminder on what necessitates a trip to the ED or clinic. See the helpful graphic below.
If you know or suspect you’re sick with COVID-19, the current recommendation is to isolate for a minimum of five days after symptom onset and remain in isolation at least 24 hours after resolution of a fever. You should still wear a mask around others until day 10. For patients that require hospitalization, it’s recommended that they stay in isolation for the full 10 days.
For many people, the virus will simply need to run its course. For those who have underlying medical conditions, such as cancer, heart disease, lung disease or diabetes, Paxlovid is an effective medication to prevent severe COVID-19 disease and works by interfering with viral replication. It’s most effective when started within five days of symptom onset.
Be Proactive, Plan Ahead
Unfortunately, respiratory virus season is upon us, and COVID-19, influenza and RSV are here to stay. Pharmaceutical (vaccination) and non-pharmaceutical (behavior modification, masking, hand hygiene, etc.) methods are the best ways to minimize risk to ourselves and others.
And don’t wait until a fever sets in to plan your next move. Talk to your primary care provider today about your eligibility for antiviral medications and other ways to help your immune system fight off whatever it might get hit with.
More Resources
- Learn more about the updated COVID-19 booster.
- Learn more about the prevention, symptoms and treatment of RSV in young children.
- When it comes to the flu vaccine, know the facts.
- Find a primary care provider that’s best for you.