Today's Medicine
Expanding Valves and Modern Care With Tried and True Technology
Published: Nov. 25, 2019

The sun is rising. The air is crisp. LeAnna MacDonald takes off on her daily walk. It won’t be the two miles she used to tackle, but after a recent minimally invasive procedure, she’s confident some of her longest treks yet are “right around the corner.”
Avoiding a “Brutal” Surgery

“I like to think I’m a pretty active and busy woman,” she said.
With a love for international travel, she and her husband have been to France, Italy and Cambodia in just the past year. Although retired, she works part-time for Millard Public Schools. Her eyes light up when she talks about the special needs students she gets to spend her time with.
“They teach me so much,” she said. “They keep me young in a sense.”
LeAnna is unique in that she’s been able to do so much while living with severe aortic stenosis – or narrowing of the aortic valve. It can cause shortness of breath, dizziness, chest pain and fatigue. Methodist Physicians Clinic cardiologist Randal Cassling, MD, monitored her condition for years. But in May, he decided it was time – LeAnna’s valve needed to be fixed.
“He said, ‘Well, it’s time we look at some options.’ That’s how he put it,” LeAnna said.
She knew open-heart surgery was one of those options, which would have been “brutal,” she said. With the lifestyle she leads, LeAnna was worried about how long and painful her recovery might be. But Dr. Cassling introduced her to another, much less invasive option – transcatheter aortic valve replacement (TAVR).
TAVR Technology
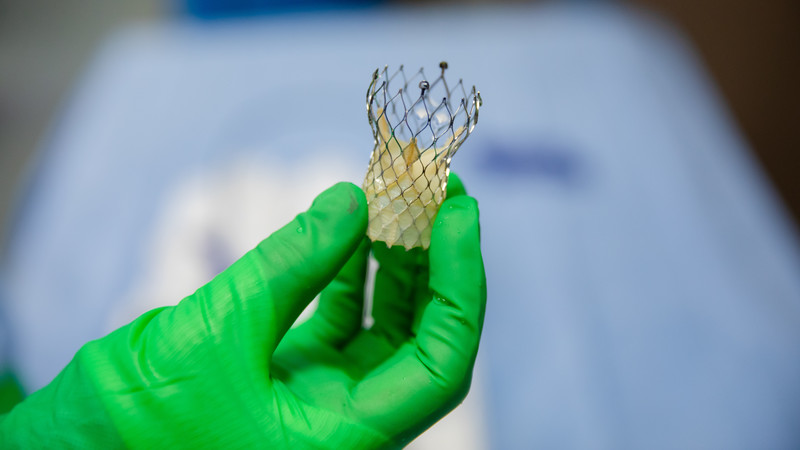
TAVR involves a small incision in the groin. A catheter is run through the femoral artery and guided toward the heart. The new valve – made up of a nickel/titanium frame and porcine heart tissue – travels through the catheter and is deployed inside the damaged valve, allowing it to expand properly. The catheter is then removed, and the incision is closed.

“That’s opposed to a six-week recovery,” said retired Methodist Physicians Clinic cardiologist Robert Hibbard, MD. “It’s really quite remarkable.”
Being deemed a candidate for such procedure was “like striking gold,” LeAnna said. She underwent TAVR in September.
Promising Results With Modern Care
While Dr. Hibbard believes open-heart surgery will always play a role in valvular disease, studies show that the global market for transcatheter therapies will likely double in the next five years.

The same can be said for other cardiac technologies at Methodist.
The WATCHMAN™ device, which was first deployed in April 2018, benefits patients with atrial fibrillation by closing off the heart’s left atrial appendage to potentially life-threatening clots.
Methodist Physicians Clinic cardiologist/electrophysiologist Matthew Latacha, MD, has performed more than 80 WATCHMAN™ procedures. Nearly every one of those patients has come off blood thinners within 45 days of the procedure.
“There is a lot of potential risk associated with blood thinners,” Dr. Latacha said. “I see people for all kinds of issues – gastrointestinal bleeding, bleeding into the brain and traumatic injuries as a result of falls. So yes, I think with WATCHMAN™ and TAVR – two procedures that fall under the category of structural heart disease, Methodist has truly reached the forefront of modern cardiology care.”
And just as Methodist continues expanding, so does its cutting-edge technology.
The CardioMEMS™ HF System – the first and only FDA-approved sensor that reduces heart failure-related hospitalizations – is something Methodist currently offers in Omaha and Council Bluffs and will be offered to Methodist Fremont Health patients by early 2020.
The paperclip-sized sensor measures increased pressure inside the lungs, which typically occurs three to four weeks before patients experience heart failure symptoms: shortness of breath, leg swelling, weight gain, fatigue and weakness. Those symptoms are often enough to land patients in the hospital.
Methodist Physicians Clinic interventional cardiologist Anand Deshmukh, MD, performs CardioMEMS™ HF procedures at Methodist Jennie Edmundson Hospital in Council Bluffs. The sensors, he said, decrease heart failure-related hospitalizations, improve the quality of patients’ lives and may help them live longer.
“Studies show that every time a patient is admitted with heart failure symptoms, they experience a decrease in heart function,” he said. “And by monitoring their lung pressure and making modifications when necessary, we are proactively preventing that.”
Not First, but Striving To Be the Best
Methodist isn’t the first health system to roll out procedures like TAVR, WATCHMAN™ and CardioMEMS™ HF, but “we pursue rigid protocols,” Dr. Hibbard said.
“We pursue all the things that are going to give us great outcomes,” he added. “Our focus is on being the best.”
“Absolutely,” Dr. Latacha said. “More important than who’s first is: Who has the best outcomes? Who has the best safety profile?”
Dr. Latacha believes that Methodist patients answer those questions every day by allowing the health system to claim the highest surgical volume in the area.
“I think that says that our hospital has a good reputation for care and that our patients trust us,” he said.
In LeAnna’s case, she was comforted knowing she wasn’t “No. 1 out of the shoot.” She’s a testament to Methodist’s Meaning of Care.
“What a gift every day is,” she said. “And that’s what Methodist gave me – many more days, many more gifts – to continue doing all the things I love. Who knows? I may have to go to Egypt now to celebrate!”
Photos and video by Daniel Johnson
More Resources
- Learn more about structural heart disease
- Read about the first patient to undergo the WATCHMAN™ procedure at Methodist
- Learn more about cardiology services at Methodist
- Read more from the Winter 2019 issue of The Meaning of Care Magazine


