Today's Medicine
Considering the COVID-19 Vaccine During Pregnancy? Here's What You Need to Know
Published: Dec. 22, 2020

As if being pregnant during a pandemic isn’t challenging enough, you’re now faced with trying to decide whether the COVID-19 vaccine is right for you.
Is it safe?
Will my baby receive some protection?
There are a lot of questions surrounding the vaccine’s safety and efficacy, and for new moms and those who are pregnant or trying to conceive, it can be confusing – maybe even scary. While there are still a lot of unknowns, here’s what we do know: All women who are eligible should consider vaccination. If I could end my plea there, I would. But the reality is not black and white.
There are several things women may want to consider before making the ever-important decision to vaccinate. The first is this: Pregnant and lactating women were not included in the Pfizer-BioNTech and Moderna vaccine trials. But based on the data from more than 70,000 participants, the vaccine appears to be safe and effective.
Understanding the Science
The Pfizer-BioNTech and Moderna vaccines are messenger ribonucleic acid (mRNA) vaccines. The mRNA is like a set of instructions for human cells to create a piece of the “spike protein” that is unique to COVID-19. You’ve likely seen this spike protein in this well-circulated image of the virus, which was released by the Centers for Disease Control and Prevention (CDC).
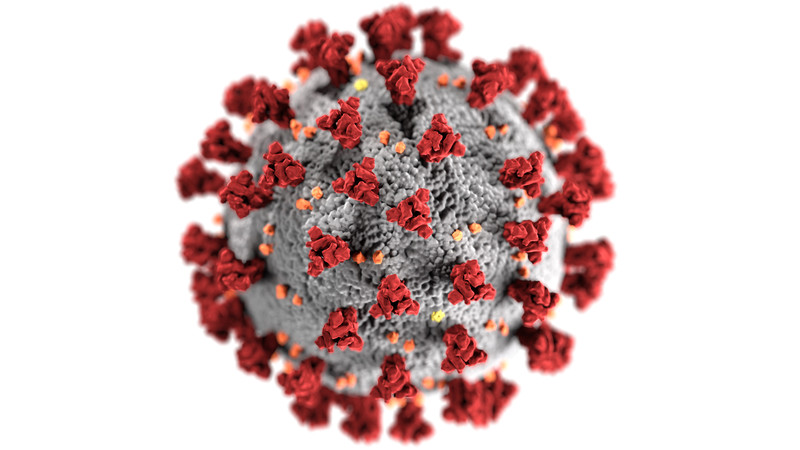
It stimulates the creation of antibodies that protect you against COVID-19. This is what makes the vaccine so effective. It does not contain the live virus or inactivated viral particles. And it cannot give you COVID-19.
However, as with many other vaccines, you may experience minor side effects, including:
- Injection site pain and/or swelling
- Fatigue
- Joint and/or muscle pain
- Fever and/or chills
- Headache
- Nausea
- Swollen lymph nodes
These side effects typically last between 24 and 48 hours. They are a normal immune system response –or a sign that your body is building immunity.
Methodist health care workers who lined up to get the
COVID-19 vaccine.
Impact on the Fetus
Once the spike protein is created inside the cell, the mRNA is immediately broken down and becomes nonfunctional. We don’t yet know whether the vaccine crosses the placenta. But if it does, that’s likely a good thing – because it would work the same in the fetus as it does in the mother, creating antibodies for protection. Additionally, there is no risk of the vaccine altering fetal DNA.
Impact on Breastfed Babies
The Society for Maternal-Fetal Medicine strongly recommends that pregnant and lactating women have access to the vaccine and that they share their decision-making with their health care provider.
Furthermore, the CDC believes that mRNA vaccines don't pose a risk to breastfed babies and that women who choose to get vaccinated don’t need to avoid breastfeeding.

Impact on Fertility
There is a widely circulated myth suggesting that the COVID-19 vaccine can cause infertility. Fortunately, it’s not true.
The antibodies created from the vaccine do not attack the critical placental protein that some have stated it could. So to be clear: There is no indication that the vaccine will cause placental malfunction or infertility.
Understanding Herd Immunity
With increasing support for the COVID-19 vaccine, the idea of herd immunity – or protection of an entire community as a result of the majority of people becoming immune to a disease – may sound promising. But herd immunity depends largely on how contagious an illness is. The more contagious a disease or illness is, the higher the percentage of vaccinated individuals needs to be before herd immunity is reached.
Scientists believe that the herd immunity threshold of COVID-19 is somewhere between 60 and 70%. But keep in mind that this can change. Even if a large percentage of people nationwide get vaccinated, there may be pockets of low vaccination numbers or a lack of community measures to prevent spread. So the best way for a pregnant woman to protect herself is to consider getting vaccinated after discussing it with her provider, and to continue social distancing, mask wearing and frequent handwashing – precautions we’ll likely need to continue taking until fall or winter 2021.
Understanding the Risk
Based on nearly a year of data regarding COVID-19 in pregnancy, we know that pregnant women are at higher risk for:
- Serious illness
- Intensive care
- Intubation
There is also evidence that suggests COVID-19 may increase the risk of:
- Hypertensive disorders of pregnancy
- Preterm birth
- Neonatal intensive care unit (NICU) admission
Based on this information, we know that pregnant women have an increased risk of serious complications with COVID-19 infection. This must be weighed against the risk of vaccination. And ask yourself:
- How likely is it that I’ll become infected with COVID-19?
- Am I health care worker, or do I work from home and follow social distancing guidelines?
- Do I have underlying health conditions like diabetes or asthma, or am I healthy?
- How far along am I?
Bottom line: If you have a high-risk profession or underlying health conditions, the vaccine’s benefits far outweigh its risks. But do talk it over with your health care provider. They’ll be able to answer your questions on a more personalized level and help you make the most informed decision possible.
More Resources
- Trust the science. Know the facts. Read up on the COVID-19 vaccine frequently asked questions.
- Learn more about the risks of COVID-19 during pregnancy.
- Follow Methodist on Facebook, Twitter and Instagram for the latest COVID-19 updates.


