Fertility Sparing Can Make Pregnancy a Reality After Gynecologic Cancer
Published: Dec. 20, 2019A gynecologic cancer diagnosis naturally brings stress, anxiety and questions: Can it be cured? How will this affect my relationship with my spouse?
For young women, there can be added worry: Will I be able to have children?
It’s often an emotional time, and some women just want the cancer gone – whatever the cost. But others are surprised and relieved to learn that with fertility-sparing options, they may not have to sacrifice having children for a good cancer outcome.
 A team approach
A team approach
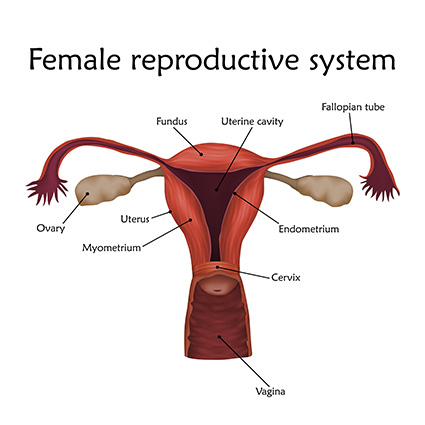
Gynecologic oncologists treat cancers of the female reproductive system – cervical, ovarian, uterine, vaginal and vulvar cancer. Most patients are close to or in menopause, so fertility-sparing conversations aren’t common.
That said, any time I see a new patient in her 20s or 30s, I make a point to find out what her fertility desires are. When a patient wants to become pregnant, I recommend bringing a reproductive endocrinologist into the conversation. We do this for a number of reasons:
- In some cases, oncological treatments can be started or continued after pregnancy
- Some treatments can make getting pregnant more difficult
- A number of options are available for women who can’t conceive naturally after treatment
Together, we can get a complete picture of the options available for cancer treatment and pregnancy.
 Fertility-sparing options
Fertility-sparing options
There are several ways we can treat gynecologic cancers with a woman’s pregnancy desires in mind. They include:
Ovarian transposition: In women who need pelvic radiation, the ovaries and fallopian tubes are surgically moved within the abdomen to protect them from radiation treatments. If they are separated from the uterus, a woman won’t be able to conceive naturally.
Radical trachelectomy: Used in some cervical cancer cases, this procedure involves removing the cervix and other tissue, then connecting the uterus to the vagina.
Unilateral oophorectomy: Often employed in cases of ovarian cancer or other ovarian problems, this procedure removes one ovary. It can be done alone or as part of a hysterectomy. A bilateral oophorectomy (removal of both ovaries) results in the inability to get pregnant naturally.
Hormonal therapy: In some endometrial cancer cases, hormone treatment (often progestins) can slow the growth of cancer or revert it to other tissue, sparing the uterus and possibly preserving fertility.
Before moving ahead, we discuss the risks, goals and expectations for treatment and possible pregnancy. The conversations we have before and after treatment aren’t always easy. Some patients aren’t good candidates for fertility-sparing options. Sometimes our best efforts can’t spare the uterus, fallopian tubes or ovaries.
Ultimately, I want patients to know that while we have many tools at our disposal, I don’t want to sacrifice a good oncologic outcome for an obstetric outcome.
Recognizing patients’ emotional needs
We understand that battling cancer and planning for children is often an emotional process. It’s important to our entire staff to provide emotional support as well as medical care. In fact, being able to help patients during these emotionally tender times is one of the things that drew me to this work.
To our staff, emotional support is a key part of a complete treatment plan. We’re committed to doing everything we can to give patients the opportunity to have children.
More Resources
- Learn more about fertility options for women with cancer
- Learn more about gynecologic oncology and reproductive endocrinology at Methodist
- Read more about Methodist cancer care and services