Simulating Poverty and Creating a System of Empathetically Aware Caregivers
Published: Jan. 21, 2020
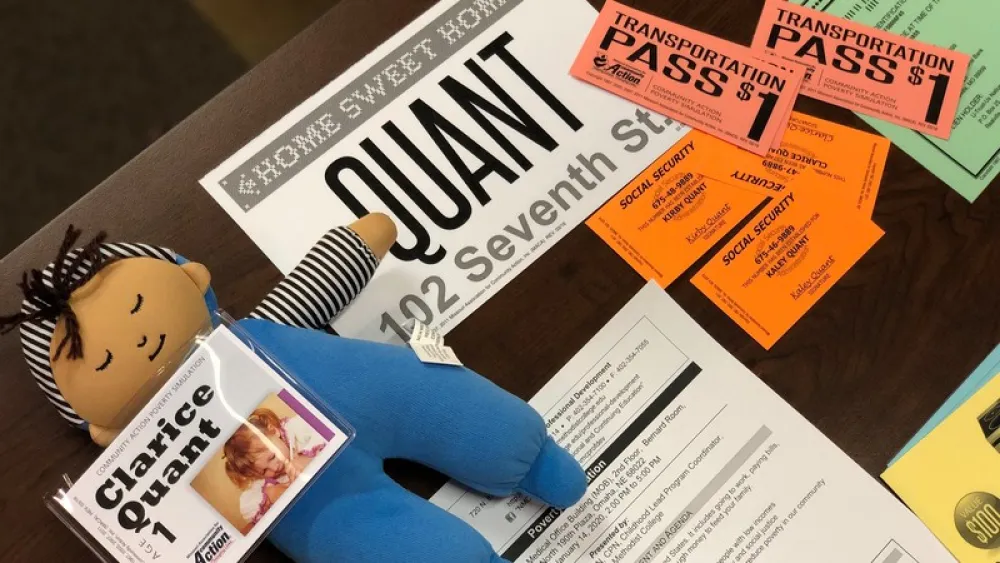
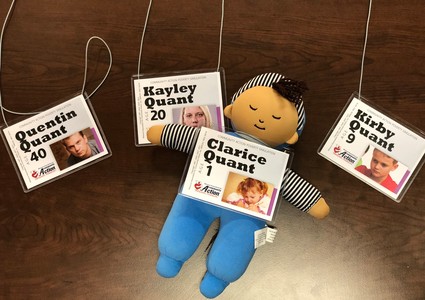
Meet the Quants: Quentin, a 40-year-old single dad who works full-time, making a little more than $1,500 a month; Kayley, his 20-year-old daughter, who’s trying to raise her 1-year-old while barely maintaining employment; and Kirby, Quentin’s 9-year-old son, who often gets into trouble at school.
They may not be a real family, but they represent a real problem that exists within our community: poverty.
Living the part
 Shon Dantzler, a medical assistant at the Methodist Community Health Clinic, was given the role of Quentin at a poverty simulation held at Methodist Women's Hospital. Darla Marriott, APRN, a nurse practitioner at the same clinic, was selected to be Kayley. And Shelley Hultman, BSN, RN, a nurse who also works at the downtown Omaha location, played the part of Kirby.
Shon Dantzler, a medical assistant at the Methodist Community Health Clinic, was given the role of Quentin at a poverty simulation held at Methodist Women's Hospital. Darla Marriott, APRN, a nurse practitioner at the same clinic, was selected to be Kayley. And Shelley Hultman, BSN, RN, a nurse who also works at the downtown Omaha location, played the part of Kirby.
In a matter of four 15-minute weeks, the Quants experienced multiple hardships, including:
- Quentin, who’d already received multiple late mortgage payment notices, ran out of gas on the way home from work and was forced to walk home in the middle of January. Even though his family was receiving food stamps, he had to visit the local payday loan store several times to feed his children.
- Kirby was suspended from school, which meant he didn’t eat much for a couple days. He was also sent to the local juvenile detention center for trying to sell a stolen stereo at a pawn shop – but at least it meant he was safe and fed.
- Kayley’s 1-year-old was taken by child protective services for neglect.
Other “families” went through similar hardships and experienced the stress and anxiety that came from strategic planning to make ends meet and, in some cases, survive.
Teri Tipton Bruening, MSN, RN-BC, CNE, vice president of patient care and chief nursing officer at Methodist Hospital and Methodist Women’s Hospital, was given the role of a single mother. She described that role as “really eye-opening.”
“My husband had left us,” Tipton Bruening explained. “I had a 17-year-old and 14-year-old. At some point, it dawned on me – I never had time to ask either of them, ‘How are you doing?’ My kids were good kids – very responsible – but that was probably not the role they should’ve been playing. Again, I didn’t have time to see if my kids were OK. It was stress-producing.”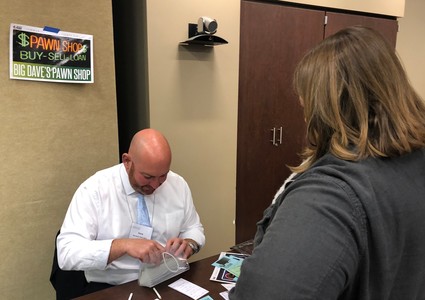
Jeff Prochazka, vice president of strategic planning and business development for Methodist Health System, played the part of a pawn shop owner. When the simulation was over, he addressed everyone participating: “I shorted every single one of you trying to sell something. I purposely miscounted the money, and I think the 9-year-old (Kirby) was the only one who caught me. It’s interesting. In the midst of such drastic measures, you ignored specifics.”
And those specifics, he explained, could have meant the difference of having enough for a meal or medication.
Addressing population health
The simulation was led by Kiley Petersmith, MSN, RN, CPEN, CPN, the Childhood Lead Program coordinator at Nebraska Methodist College and a former Emergency Department (ED) nurse.
“Working as an ED nurse, I saw so many families come in with non-emergent issues,” she said. “You wonder, ‘Why is this parent coming in with a child who appears to have a common-cold fever?’ But you quickly realize that they don’t know what else to do. They know their child hasn’t been getting proper nutrition because they live 10 miles from a grocery store. They don’t have money for medication. They can’t afford to drive anywhere else. And they’re scared. They don’t want to be turned away.”
 While Petersmith’s job is to educate and influence future health care workers, she realizes that those currently working in health care need this type of awareness, too.
While Petersmith’s job is to educate and influence future health care workers, she realizes that those currently working in health care need this type of awareness, too.
“It promotes empathy,” she said. “And it makes us better as a health system. By living the part – not just being told poverty exists – we might be inspired to find the root cause of our patients’ health issues and direct them to the resources they need. We might be able to focus on primary prevention – keeping people healthy rather than just putting a Band-Aid on after the fact.”
Things like life expectancy, infant mortality and incidences of chronic disease in the Omaha area can all be estimated by ZIP code, Petersmith said. It’s a big part of population health – a concept that addresses the health outcomes of various groups of people locally.
“Let’s say you look at areas of high lead exposure and ask yourself, ‘Why?’ A little research will show you, ‘Oh, those areas are also inundated with old housing.’ How many of us are asking patients things like, ‘Do you have mold in your home? Cockroaches? What’s the air quality like where you live?’ We are failing populations if we’re only asking about their symptoms.”
Creating change
Poverty simulations are one of many ways Methodist is coming together as a system to create change.
“While we wish we could spend 60 minutes with each and every patient, we can’t,” said Amanda Williams, director of population health for Methodist Health System. “So, we’re working to formulate better trigger questions – questions we can ask patients during the time we do have with them – that might lead them to open up about the challenges they’re facing.”
Methodist is considering a community paramedicine model, which focuses on community-based health care in a way that enhances access to primary care and reduces health disparities.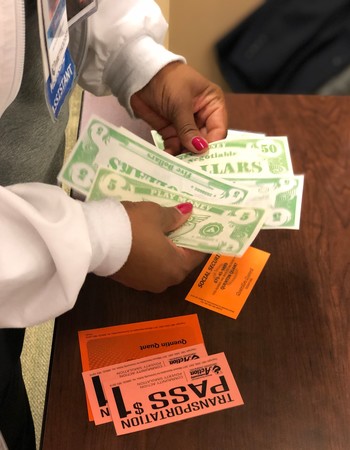 And the online tool, Aunt Bertha, is something else the health system is currently exploring, especially for use among nurses, to help patients identify resources by ZIP code.
And the online tool, Aunt Bertha, is something else the health system is currently exploring, especially for use among nurses, to help patients identify resources by ZIP code.
The simulation, which drew 42 voluntary participants, was a first for Methodist employees. But Williams and Petersmith are confident it won’t be the last.
“It’s about breaking down barriers and biases,” Petersmith said.
The most important takeaway, she believes, reestablishes this: No matter their income, everyone deserves quality care. Everyone deserves to experience The Meaning of Care.
More Resources
- See WOWT's coverage of a poverty simulation for Nebraska Methodist College students
- Read more about Kiley Petersmith’s perspective on poverty simulations and the importance they play in health care