





Family Health
‘So Much More Than Growth Charts’: After Spotting Rare Condition, Methodist Pediatrician Stresses Importance of Well-Child Visits
Published: Nov. 21, 2022

The first time Allison Warren was introduced to pediatrician Emily Bendlin, MD, was at her son Wade’s 2-month well-child visit – shortly after his initial pediatrician had moved out of state.

“I laid him down on the exam table, and Dr. Bendlin started looking closely at his forehead,” Allison said. “She started pointing out various features of it – like that his temples were dimpled. I personally had noticed that, but I didn’t realize that it meant anything was wrong.”
It’s a difficult conversation to have with new families, Dr. Bendlin said: “That, ‘Hi, nice to meet you. I think there’s maybe something that needs addressing.’”
But making those conversations as comfortable as possible is an important trait of a pediatrician, she said. So Dr. Bendlin took her time with Allison, showing her Wade’s bulged forehead, comparing it to photos on her computer and pointing out the feeling of a prominent ridge down the middle of his forehead.
“Mom to mom, she really took the time to explain everything to me,” Allison said.
Early Intervention
Wade was eventually diagnosed with metopic craniosynostosis.
“It just rolls off the tongue, right?” Dr. Bendlin said, using light-hearted sarcasm to illustrate how complicated and scary a diagnosis like that probably sounds to the average parent.
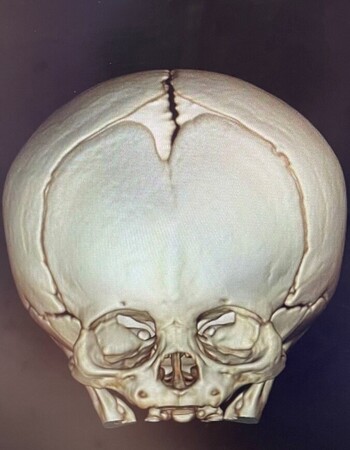
She explained the condition as she explained it to Allison: “A baby’s skull has lots of small bones that are separated by growth plates called sutures. The metopic suture, which is the suture that runs down the forehead of a baby, is the suture that fuses the earliest. But if it fuses too early, it can cause issues in terms of appearance and brain development later in life.”

Because Wade’s rare disorder was identified early, he was eligible for an endoscopic craniotomy – a minimally invasive procedure in which an endoscope is inserted through a small incision in the forehead to cut out the fused portion of skull. It’s typically done between 3 and 4 months of age to ensure a successful outcome.
“If we would have held off on that 2-month appointment, or if Dr. Bendlin hadn’t noticed it until he was a little older, he would have needed a total cranial reconstruction,” Allison said.
“And that would have been a lot more invasive,” Dr. Bendlin said. “A lot more risk and potentially a much longer recovery.”
Every Visit Matters
Wade’s procedure in early November went flawlessly. He’ll now wear a helmet for up to a year to help mold his head into a more normal shape.

According to Dr. Bendlin, this was the best possible outcome.
“Oh, my goodness, my nurses and I have been so invested in this,” Dr. Bendlin said. “So being able to experience the excitement of a good outcome for them is so wonderful. It’s really, really rewarding.”
But she takes little credit, knowing it was Allison’s diligence in adhering to her son’s well-child care schedule that paved the way for his well-being. Even if a child checks out fine one month, Dr. Bendlin said, the same can’t be guaranteed the following month.
“Kids go through their most rapid periods of growth in those first two years of life,” she said. “And not just in terms of physical growth, but also in brain development. That’s why Wade’s story is such a good example of what can be missed by the naked eye. There are several things we’re trained to pick up on as pediatricians that might be so subtle most parents or family members wouldn’t ever notice.”
A Team Approach
Well-child visits are “about so much more than growth charts,” Dr. Bendlin said. She uses every visit to conduct “developmental surveillance” – or look at a patient’s physical traits as well as what they’re saying and doing.
“We’re constantly looking at and for certain things even when parents don’t necessarily notice we are,” she said.
But Dr. Bendlin is well aware that one visit alone can’t possibly provide a perfect snapshot of a child’s overall health.
“And I think that highlights the importance of parental involvement,” she said. “Because it’s not uncommon for a child to be very shy and not talk to me at all during the visit. That’s where it’s really important to get as much information as possible from parents – whether it’s through the questionnaires they fill out or the concerns they feel comfortable bringing up at their visits.”
It takes a team approach in pediatrics – a branch of primary care, which is one of five specialties that Methodist Health System truly excels in – she said.
“And I would attribute that to our pediatricians really taking these families on as our own,” she added. “Making these families feel like we’re their medical home and really working closely with them and other staff to provide the best outcome possible for their child.”
It’s The Meaning of Care, she said. And according to Allison, it’s everything Dr. Bendlin stands for.
“She’s relatable, she’s thorough, and I’m so grateful she’s ours.”


