Today's Medicine
Older Adults and the COVID-19 Vaccine: Adjusting to Changes and How Loved Ones Can Help
Published: March 10, 2021

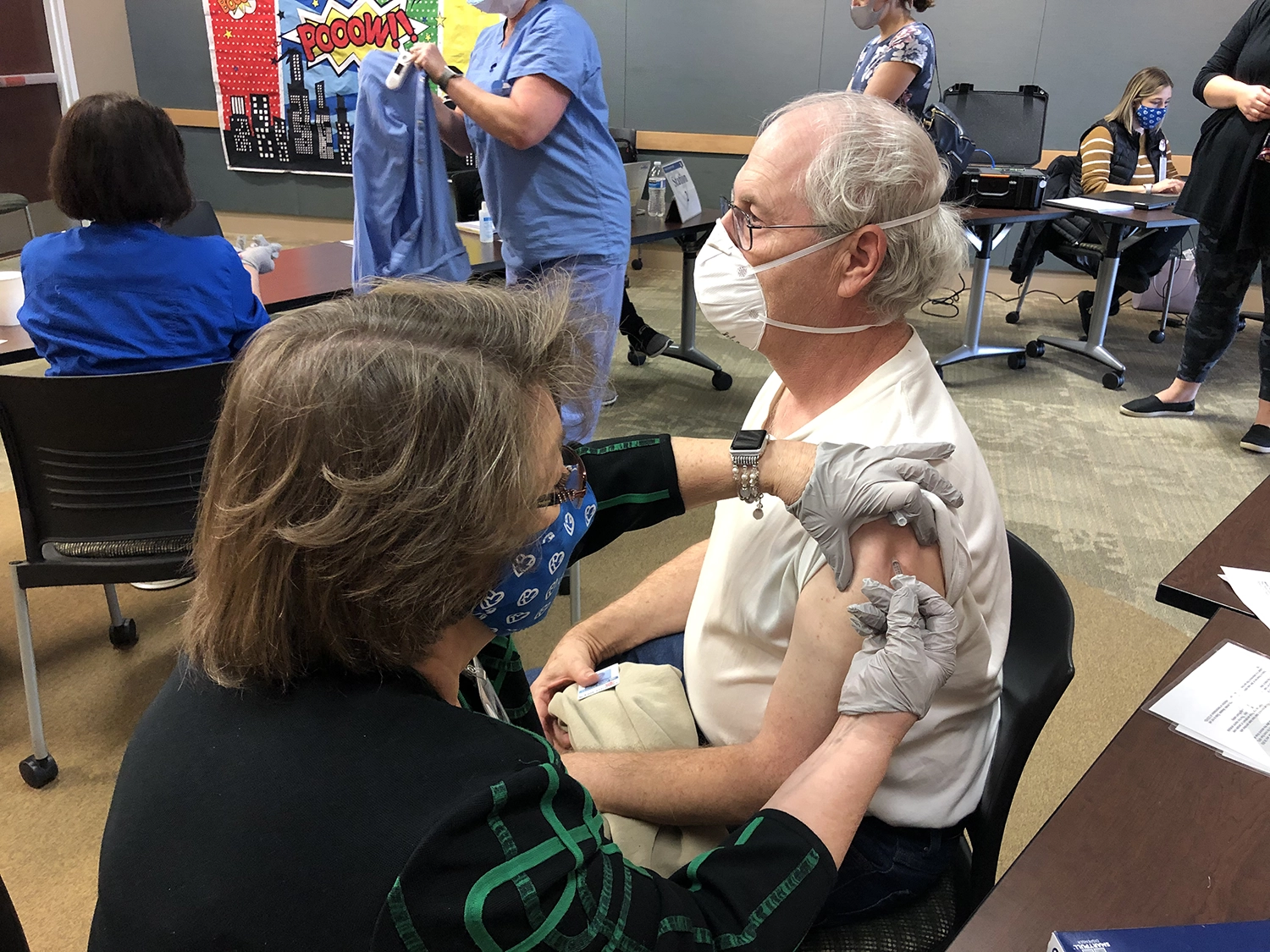
As more adults age 65 and older get vaccinated for COVID-19, their lives can begin to open up again. Those steps forward will still need to be done cautiously while following guidelines from the Centers for Disease Control and Prevention (CDC), but some of the stress and isolation that many older adults have been experiencing during the COVID-19 pandemic can begin to ease.
Whether you’re an older adult who still has questions about the COVID-19 vaccine or you’re a family member worried about cognitive changes in an older relative, this next year is going to be filled with a new set of challenges.
Frequently Asked Questions
I’m over the age of 65. Why should I get the vaccine?
Older adults have been hit the hardest during the pandemic. According to the CDC, eight out of 10 COVID-19 deaths in the U.S. have been among adults age 65 and older. There’s a reason this age group has been prioritized for vaccination across the country.
Headlines about vaccine effectiveness get confusing. What do I need to know?
The great news is that all currently available vaccines have been proven to be effective in preventing serious illness and death from COVID-19. That message sometimes gets lost in headlines or debates over which vaccine is better. Here’s the bottom line: Research shows that taking any approved vaccine when it’s offered to you can save your life and help end this pandemic.
If I get vaccinated, why do I still need to mask?
Even after being vaccinated, you still need to practice masking, social distancing and good hand hygiene. There are many unknowns regarding variants and whether a vaccinated person can still contract and spread COVID-19. Studies show you’re protected from severe outcomes, but you don’t want to risk infecting someone else who is still waiting for their turn to be vaccinated.
I’m worried about experiencing side effects. What should I expect?
Those side effects you’ve been hearing about are appropriate immune responses – signs your body is building immunity. Read about common side effects and how to minimize them, and talk to your family and friends who’ve been vaccinated so you know what to expect.
I reached out to some of my Methodist colleagues age 65 and older to share their experiences:
Karen Lauer-Silva, MD, OB/GYN at Methodist Physicians Clinic Women’s Center: “I had very mild symptoms. I had some tenderness at the vaccination site that lasted about two days and was essentially the same for both doses. I had some body aches and muscle soreness that started about Day 3 and lasted for a couple days. I was somewhat fatigued for about a week total with each vaccine – the fatigue was greater with the first dose than the second. But I never had symptoms that prevented me from doing my usual activity, including full-time work. I wanted to be vaccinated to protect the people in my world: my patients, my family and my socially distanced church family!”
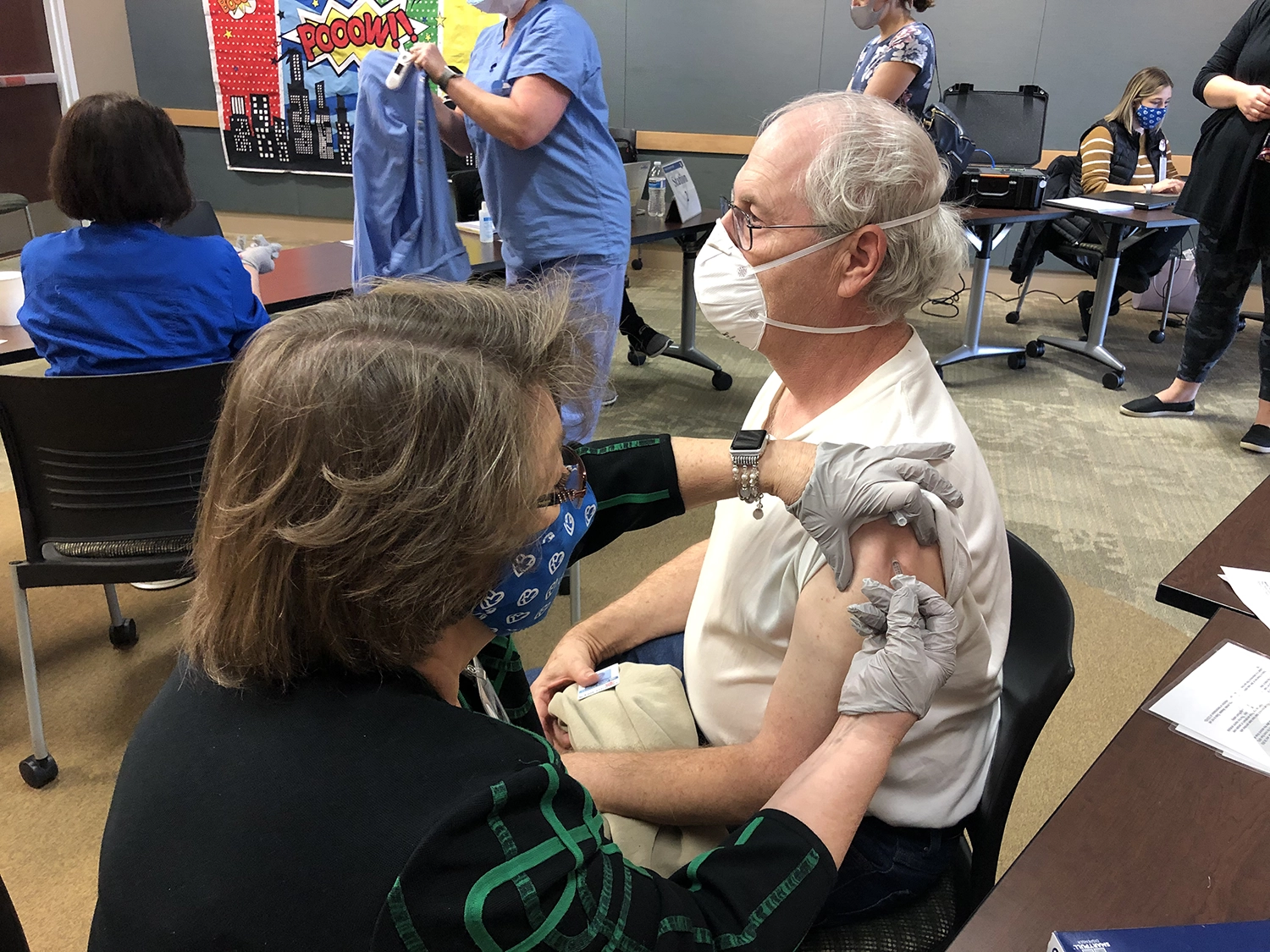
Thomas Seidel, MD, Neonatologist at Methodist Women’s Hospital: “I had moderate soreness in my shoulder starting about four hours after my first dose. The pain was gone within 24 hours, and I didn’t take any pain medication. After the second dose, I had moderate soreness in my shoulder again, and it was somewhat worse than the first dose. It lasted about two days, and again, I took no pain medication. I had no fever, fatigue or headache. I got the vaccine to protect myself. My age puts me in that high-risk category.”
John Lohrberg, MD, Family Medicine Physician at Methodist Physicians Clinic: “I was infected with COVID-19 in the fall and received my first vaccine 90 days after my positive test. After the first dose, I experienced some mild muscle aches and chills and felt clammy for a couple days. This was easily treated with ibuprofen. I didn’t notice any other side effects. I was prepared for a more significant response after the second dose, but it was actually milder – I didn’t really have any side effects. I was happy to get vaccinated because over the years, vaccinations have been shown to be the best way to prevent illness. I’ve never had any issues with vaccines and have had only a few patients with significant but not life-threatening or long-term reactions to vaccines in my over 30 years of practice. I’m a supporter of all vaccinations.”
I got my second dose, but I’m still too nervous to even get together with other vaccinated friends. Is that normal?
In early 2020, you wouldn’t have thought twice about having dinner with family or friends, attending a celebration or running an errand. It’s understandable – and expected – that you may have mixed feelings about resuming certain activities once it’s safe to do so. By now, you’ve spent a full year calculating the risk of every situation and perceiving crowds and close contacts as risks. So it may take time to feel more comfortable engaging with others and venturing outside the home.

How can I start feeling more comfortable, especially around other vaccinated people?
Research generally suggests that it can be helpful to ease your way into such big adjustments. Some advice to keep in mind:
- Be patient with yourself as you adjust to new routines and activities.
- Go at a pace you’re comfortable with. When you feel ready, gradually add in activities that are safe to resume.
- Remember that it’s not a race. Just because a friend is ready to go back to your fully vaccinated book club, doesn’t mean you should feel bad if you’re not there yet.
Your life after the vaccine will be another period of change, but this time the focus is on getting back to what you’ve been missing over the past year – the relationships and activities you find most meaningful. Talk with people you trust, like your family, caregivers or health care providers. They can provide a sounding board to process emotions you may experience and help determine a plan for easing back into society that makes sense for you.
My mother has stayed fairly isolated this year, but she’s vaccinated now. I’m worried that I’ve missed cognitive changes. What should I look out for?
Given that many older adults have had more limited interaction with friends and family over the past year, it’s possible that some cognitive changes may have gone unnoticed. Family members, caregivers or close friends are often the first to raise concerns that an aging adult is starting to have changes in memory, thinking or mood. When more regular interactions resume, family and friends may have more of an opportunity to identify cognitive changes that may be subtle and harder to spot during brief visits or over the phone.
Cognitive changes to watch for include:
- Changes in behavior or hygiene
- Inability to manage complex responsibilities, like remembering to pay bills, remembering to take medications or managing household tasks
- Repeating stories or questions
- Forgetting recent experiences or conversations
- Confusion
- Decreased interest or motivation in activities
If there’s a concern about changes in thinking, personality, behavior or general functioning, contact a health care provider. We’re here at the Methodist Geriatric Assessment Clinic to help as well.
I’m still on the fence about getting the vaccine. What should I do?
Please reach out to a trusted health care provider if you have questions or concerns about the COVID-19 vaccine. And seek out reliable information – from health systems, local newspapers and television stations, and the CDC website.
More Resources
- Get answers to more questions about life after the COVID-19 vaccine.
- Learn more about how to minimize common COVID-19 side effects.
- Considering the COVID-19 vaccine during pregnancy? Here's what you need to know.
- Follow Methodist on Facebook, Twitter and Instagram for the latest COVID-19 updates.