Cancer Care
CAR T-cell therapy at Methodist provides a 'curative' sense of hope
Published: Nov. 7, 2024
Chemotherapy. Radiation. Immunotherapy.
Many lymphoma patients might assume those are their only treatment options.
But a new, state-of-the-art therapy that’s proven wildly successful at Methodist, is infusing a renewed outlook into many patients who previously saw little to no success with other treatment modalities.
How it works
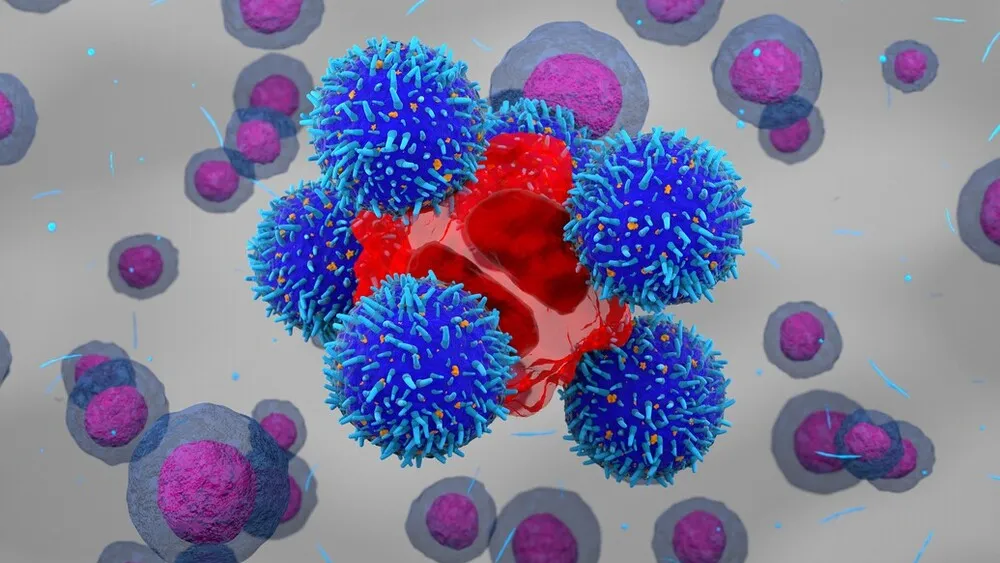
CAR T-cell therapy involves the extraction of a patient’s T cells – white blood cells that fight infection or illness – for the purpose of reengineering them with chimeric antigen receptors (CARs) that bind to a protein on cancer cells. The infusion of those modified T cells back into the patient’s bloodstream is where the magic happens, as those CAR T cells get to work on targeting only the cancer cells – not healthy cells.
Methodist Hospital, the first community-based hospital to offer CAR T in the region, spent two years researching the technology, creating policy surrounding administration of the treatment and training staff before offering it to its first patient in May 2024 – a woman in her 20s battling recurrent lymphoma – who’s now in remission.
“It’s not just getting a couple oncologists and nurses trained,” said Joel Michalski, MD, PhD, a Nebraska Cancer Specialists hematologist and oncologist, who oversees the care of CAR T patients at Methodist. “There are probably hundreds of hours that need to be invested by a hospital in order to become an authorized site for this. And honestly, outside of Methodist and Nebraska Medicine – the two entities that offer this kind of therapy in Omaha – I don’t know that there’s any other health system in the region that would be able to navigate such a feat.”
Side effects
What’s touted as more effective than chemotherapy in certain cases isn’t for everyone. Methodist currently offers CAR T therapy to lymphoma – and, soon, multiple myeloma – patients whose disease relapsed or wasn’t responsive after a previous therapy, like chemotherapy. And although CAR T candidates may not lose their hair like they can with chemo, there are other common side effects, including fever, nausea, low blood pressure, rapid heartbeat, difficulty breathing and neurotoxicity, which affects the central and/or peripheral nervous system.
At Methodist, patients are hospitalized for up to two weeks after their CAR T-cell infusion while a specialized care team monitors them for complications.
“It could be a change in their handwriting, aphasia – where they can’t quite find the right word – or overall confusion,” said Lisa Schraufnagel, Methodist Hospital’s oncology service leader. “More serious complications would be seizures or brain swelling. But keep in mind, a patient may still be safe to discharge even if they experience low-grade neurotoxicity.”
It’s a small price to pay, according to Methodist’s CAR T recipients and specialists, for a one-time treatment that has what Dr. Michalski calls a “curative intent.”
A renewed sense of hope
“The results we’re seeing are providing a sense of hope to patients who might otherwise not have it,” Schraufnagel said.
And that hope, Dr. Michalski believes, is even greater when it’s found close to home.
“Patients should not have to deal with the stress of traveling to a giant, unfamiliar health system to get excellent oncology care,” Dr. Michalski said. “And I think that’s one of the best kept secrets about Methodist and our partnership with them. Not only are our patients able to get cutting-edge cancer care, but we’re offering as many – if not, more – clinical trial options than larger, reputable facilities outside of Omaha. And that’s where I feel we’re going next with CAR T. I see us becoming a trial site in using this kind of technology for all forms of cancer – not just blood malignancies – and having the opportunity to help even more patients.”
More Resources
- Read more from the fall/winter 2024 issue of The Meaning of Care Magazine.
- Learn more about cancer care services at Methodist.


