
The Meaning of Care Magazine
'This Job Makes a Difference': Methodist Pathology Center Makes an Impact Behind the Scenes
Published: April 10, 2023
Methodist Physicians Clinic pulmonologist Adam Wells, MD, cares for patients with a variety of respiratory conditions, including pneumonia, COPD, COVID-19 and lung cancer. But even with his years of experience, a patient’s diagnosis and treatment plan aren’t always obvious.
That was the case when Janelle McCormack visited him last spring. Janelle went to the Methodist Hospital Emergency Department a week earlier and was admitted after experiencing shortness of breath and chest pain.
“To me, it seemed like it was out of the blue,” the retired nurse said.
She was treated with steroids to address her acute symptoms, discharged on oxygen, and referred to Dr. Wells for follow-up care.
What he found – or didn’t find – was puzzling. Janelle has rheumatoid arthritis, an autoimmune disease known to sometimes cause lung problems. Imaging and lab work ruled out blood clots, pneumonia and other infections.
“But the lab work wasn’t really conclusive about what was going on in her lungs,” Dr. Wells said. “This was much more complicated than the typical pneumonia.”
He now suspected interstitial lung disease, a term for any of several conditions that can damage the lungs. While the conditions aren’t common, people with autoimmune diseases are at more risk to develop them.
In Janelle’s case, Dr. Wells needed a lung biopsy to determine her condition – a recommendation he didn’t take lightly.
“Bronchoscopy is an option for biopsies, but she was sick enough and had a funny enough story that I thought we needed to get a bigger tissue sample,” he said.
After discussing her options with Dr. Wells, Janelle agreed.
“I was kind of hesitant to do that,” she said. “I tried to avoid surgery, but I felt like it was important that they have that information to better understand how to treat me.”
Dr. Wells was about to lean on the lab again.

Passionate About Medicine
The Methodist Pathology Center-Schenken Pavilion’s main building on the Methodist Hospital campus is hidden in plain sight, nestled to the south of the patient and visitor parking garage. With a laboratory on the Methodist Women’s Hospital campus as well, the center has over 200 staff members and performed over 1.9 million tests in 2022 in its clinical labs, which primarily test samples of bodily fluid, and anatomic labs, which focus on tissue samples.
The center also serves Methodist Physicians Clinic locations; collaborates with labs at Methodist Fremont Health and Methodist Jennie Edmundson Hospital; and is a regional leader, providing services to hospitals, clinics and other facilities throughout Nebraska, Iowa and Missouri.
It’s the kind of often unseen collaboration that makes modern health care possible.
“Doing our jobs well helps doctors get that accurate diagnosis faster, which gets patients their treatment faster,” said Allison Sperry, MHA, HTL(ASCP)CM, the center’s team leader for histology. “The people in the lab have a real passion for the medical field. We’re not all the type who can personally care for patients, but we can do it behind the scenes.”
“We have something to do with just about every patient,” added pathologists’ assistant Mark Pemberton, PA, (ASCP)CM. “Not every department can say that, and that’s kind of neat. Even though we don’t see patients, we have an effect on their treatment, ideally.”

for a pathologist’s examination.
No Room for Error
A specimen’s journey through the lab is defined by precise steps with no room for error. They arrive via courier and first go through a control process meant to verify what patient they came from and how they’re to be tested. Many clinical pathology tests – COVID-19, blood and urine tests, for example – are performed on specialized machines operated by lab scientists. Janelle’s case, meanwhile, required the experts in the anatomic lab.
After reviewing Janelle’s CT scans with Dr. Wells, Methodist Physicians Clinic thoracic surgeon Karin Trujillo, MD, opted to perform robotic-assisted surgery. Using this minimally invasive approach, she removed two small wedges of Janelle’s left lung – one sample of damaged tissue and another of healthy tissue.
At the pathology center, such tissue is dissected by pathologists’ assistants in the first step toward creating slides for examination under a microscope. Using their knowledge of organ systems and disease progression, they work to identify the parts of the tissue that can best help a pathologist make a diagnosis.
“The small specimens, like moles and gastrointestinal tissue biopsies, are relatively easy to process,” Pemberton said. “But when you have an entire lung or an entire organ, or three feet of colon, it’s not practical to look at that entire specimen under the microscope. My job is to determine what questions need to be answered with the minimal amount of microscope slides.”
From there, the histology team steps in, treating the selected tissue sections with a variety of chemicals and reagents to remove moisture, prevent decay, increase their transparency and stabilize them. This results in paraffin wax blocks that can be thinly sliced and placed onto slides for examination. Stains applied to the slides can enhance a pathologist’s view of the tissue and in some cases interact with diseased or damaged tissue to aid in a diagnosis.
While examining Janelle’s lung tissue, pathologist John Gentry, MD, the center’s director of anatomic pathology, knew he was trying to identify an interstitial lung disease. Still, he said, “This wasn’t a perfect textbook case.”
“These are not the most common specimens to see, and they are difficult because each disease has a constellation of findings that you’re looking for,” he said. “A lot of findings you might have overlap with other diseases. It can be very tricky.”
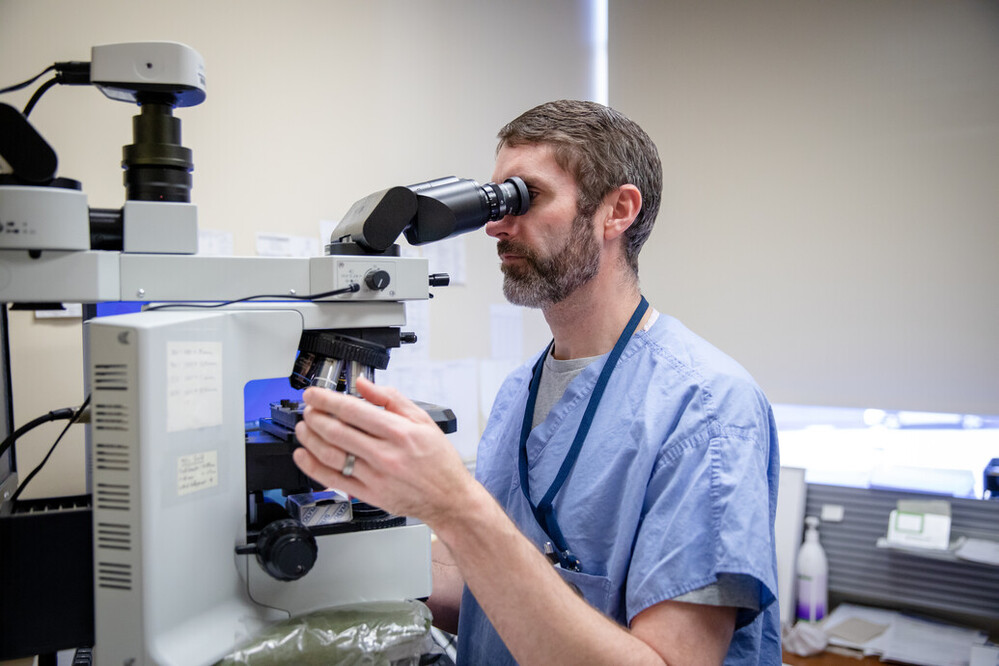
The wrong diagnosis could result in the wrong treatment, so Dr. Gentry sought a second opinion. He sent slides of Janelle’s lung tissue to an expert in interstitial lung diseases at the University of Michigan – a common practice in the world of pathology.
“Anytime you run into a case where you just can’t figure it out, or it’s really rare, or it’s the first time you’ve ever seen it, we send it out,” Dr. Gentry said.
The result: Janelle likely had hypersensitivity pneumonitis, an allergic reaction that causes inflammation and can damage the lungs.
“Something To Celebrate”
Armed with more information about what was causing Janelle’s issues – and what wasn’t – her care team could proceed with a more defined treatment plan, including corticosteroids prescribed by Dr. Wells, immunosuppression medication prescribed by her rheumatologist to reduce lung inflammation and pulmonary rehabilitation.
“Without knowing more about her interstitial lung disease, you could really hurt her by giving her a certain treatment,” Dr. Wells said. “After that biopsy, we changed treatment plans accordingly, and now she’s off and living again.”
A year later, Janelle is no longer on oxygen, she’s completed pulmonary rehab, subsequent CT scans show only a small amount of lung scarring, and her pulmonary function tests show significant improvement. More important, she’s spending her time how she wants – attending exercise classes, visiting friends and enjoying her children and grandchildren.
“It’s just been smooth sailing,” Janelle said. “I’m grateful that I feel this well. Until you’re faced with something like this, you never think it’s going to happen to you.”
The team effort that led to her recovery isn’t lost on her.
“I know from being a retired nurse that there’s a lot more that goes into it than just taking the biopsy and surgery,” she said. “I think that sometimes we just think it’s magic behind the scenes, but there are people working hard so the pathologist can make a determination of what’s going on.”
Sperry said that knowing they’re part of outcomes like Janelle’s is humbling for her and her colleagues.
“You’re like, ‘Wow. I really did help somebody’s loved one. And I hope somebody in the same role as me helps my loved one someday,’” she said. “It’s something to celebrate. This job makes a difference.”
Photos and video by Daniel Johnson and Nick Bohan
More Resources
- Read more from the spring 2023 issue of The Meaning of Care Magazine.
- Learn more about the Methodist Pathology Center-Schenken Pavilion.
- Read more stories about Methodist's commitment to cutting-edge medicine.


