The Meaning of Care Magazine
Medication Reconciliation Enhances Patient Safety in Hospital and After Discharge
Published: April 10, 2023
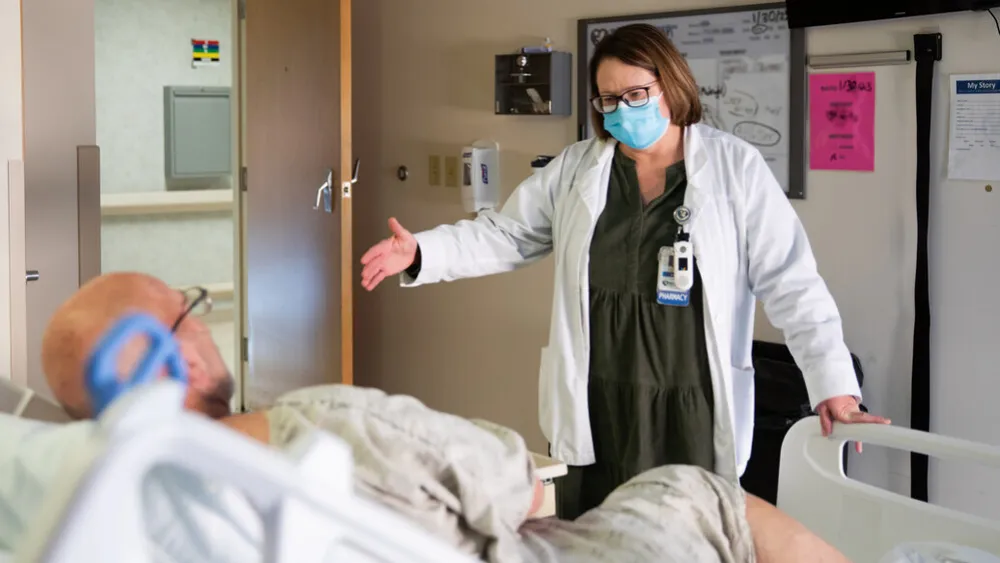
Patient care pharmacist Paula Chicoine checks in with a patient at Methodist Jennie Edmundson Hospital.
Rose Pangburn doesn’t remember the first few days of her stay at Methodist Jennie Edmundson Hospital in December. But she’ll never forget the result of her care – and how it extended past her discharge.
Rose was rushed to the hospital in Atlantic, Iowa, then transferred to Jennie Edmundson on Dec. 1 after experiencing intense back and abdominal pain, the result of a gallstone and an infection in her gallbladder. On the ambulance ride to Council Bluffs, her blood pressure took a dive.
The last thing she remembers is talking to a hospital nurse about her living will, then praying. When she woke up several days later – on a ventilator and with her family surrounding her – she learned she had gone into cardiac arrest before the surgery could take place.
“I’m just lucky to be alive,” said Rose, a retired nurse. “I have nothing but high praises for every staff member in that facility that took care of me. I got top-notch care.”
The staff’s care continued for 11 days and, to her surprise, after she arrived home.
Just hours after leaving Jennie Edmundson on a Sunday, Rose took a call from patient care pharmacist Paula Chicoine, BSPharm, RPh. While reviewing discharge information, Chicoine had noticed discrepancies with Rose’s prescriptions. Chicoine was calling to check if Rose had picked up her medication – she hadn’t yet – and walk her through a few changes.
“I’ve never had anybody do that before,” Rose said. “Calling like that to go over meds and making sure I understood and that everything was right, that impressed me.”

An Important First Step
Chicoine’s review of Rose’s prescriptions is just one part of medication reconciliation – a largely behind-the-scenes effort at every Methodist hospital that adds a layer of protection for patients throughout their stay and after discharge. While staff members are continually reviewing patients’ medications during hospitalization, they’re also paying particular attention during a patient’s admission and as discharge nears.
“Transitions of care have become an area of great vulnerability for patients, and the biggest transition patients make is when they leave the hospital and either go home or to another facility,” said Angela Elam, PharmD, a patient care pharmacist at Jennie Edmundson. “It’s a time in which unintentional errors or miscommunication can occur. What we want to do is maximize medication management for our patients, reduce readmissions and improve the health of our patients in our community.”
A successful hospital stay and discharge begin with verifying a patient’s medication history at admission – a process that can be straightforward or require a little detective work.
Katie Goodwin, CPhT, a certified pharmacy technician specialist at Methodist Hospital, routinely accesses patients’ electronic medical records and pharmacy records. If a patient is being transferred from another facility, its records also will often include medication information. And perhaps Goodwin’s most powerful tool: talking with a patient and their family, which involves more than just asking for an up-to-date medication list.
Goodwin and technicians across Methodist are gathering as much information as they can to set up the patient and hospital staff for success. A complete medication history can help pharmacists and providers continue a patient’s necessary prescriptions, stop doses that aren’t beneficial during their hospital stay and make adjustments to avoid negative interactions with new medications. It’s also not uncommon for technicians to identify patient errors such as taking the incorrect dose of medication, continuing to take medications they no longer need or neglecting to take ones they do.
In Rose’s case, Jennie Edmundson staff had plenty of information to work with when she arrived. They were able to access medication information gathered at the hospital in Atlantic, and her family shared the medication list she carries with her.
“I feel like it gets patients off on the right foot at the hospital,” Goodwin said. “Through those lines of questioning, of verifying medications, when last doses were taken and how a patient is taking meds, it can bring forward those potential issues. And then the doctors better know what to do and how to treat from there.”

Collaboration Is Key
A medication history helps lay the foundation for a safe hospital stay, but seeing it through requires a team effort. That includes the help of pharmacists, who are continually reviewing each patient’s evolving situations and medications, then consulting with providers.
“Nowadays, there’s just an explosion of new meds,” said Jennie Edmundson hospitalist Evelyn Reher, MD, who’s been practicing for over 25 years. “Just by sheer number, you know the major interactions, but you can’t know every single medication in the specialty fields and their total side effect profile. The pharmacists give us that information to keep the patient safe. I have someone who has my back.”
Meanwhile, work is underway throughout a patient’s stay to ensure a safe medication regimen after discharge. Nurses, providers and pharmacists may be involved in patient education, and there are also frank discussions with patients and families about how they’ll obtain their medications.
“We really want them to understand the med they’re on, why they take it and the side effects, if any,” Elam said. “We collaborate with the physician, nursing staff, social work and other people on our interdisciplinary team to identify medication barriers, such as access or cost, and find solutions. We want to address anything that would hinder the patient from being able to get their medications and take them appropriately.”
As discharge nears, pharmacists are busy verifying and updating medication information that will be included in a patient’s record and sent on to pharmacies, primary care providers and other care facilities, if necessary. Just as medication reconciliation efforts at admission help ensure a safe hospital stay, the work at discharge prepares patients for the best outcomes after they leave.
“I’m getting a good handoff, and it’s a big deal to me and the patient,” said Luke Lansman, MD, a family medicine physician who cares for patients at Methodist Physicians Clinic in Fremont. “Taking care of someone after they’ve come out of the hospital, it’s good to know exactly what was changed and why. Rather than spending time figuring out what changes have been made, I can spend that time helping them better understand them and any adjustments or monitoring that need to be made.”

Care Beyond the Hospital Walls
One discrepancy Chicoine identified during her final review of Rose’s prescriptions was that an order hadn’t been sent to her pharmacy. The simple phone call that followed wrapped up a hospital stay defined by quality care, Rose said.
“It gave me peace of mind,” she said.
Said Chicoine: “It’s a small thing, but if you can help one patient, you’ve done a good thing. It’s a very satisfying part of my job.”
But she’s quick to point out that she’s not alone. She and her colleagues know that across Methodist, medication reconciliation is a team effort aimed at keeping patients safe and healthy.
“This is why we do what we do,” Elam said. “Everybody can’t know everything, including us and including the physician. We’re all working together to make sure that our patients get the best care they can get.”
Photos by Nick Bohan
More Resources
- Read more from the spring 2023 issue of The Meaning of Care Magazine.
- Read more stories about Methodist's commitment to cutting-edge medicine.