Inspiring Stories
Occupational Therapists: Using Compassion and Creativity To Address the Needs of COVID-Positive Patients
Published: April 14, 2021
When it comes to occupational therapy, there may be a few misconceptions.
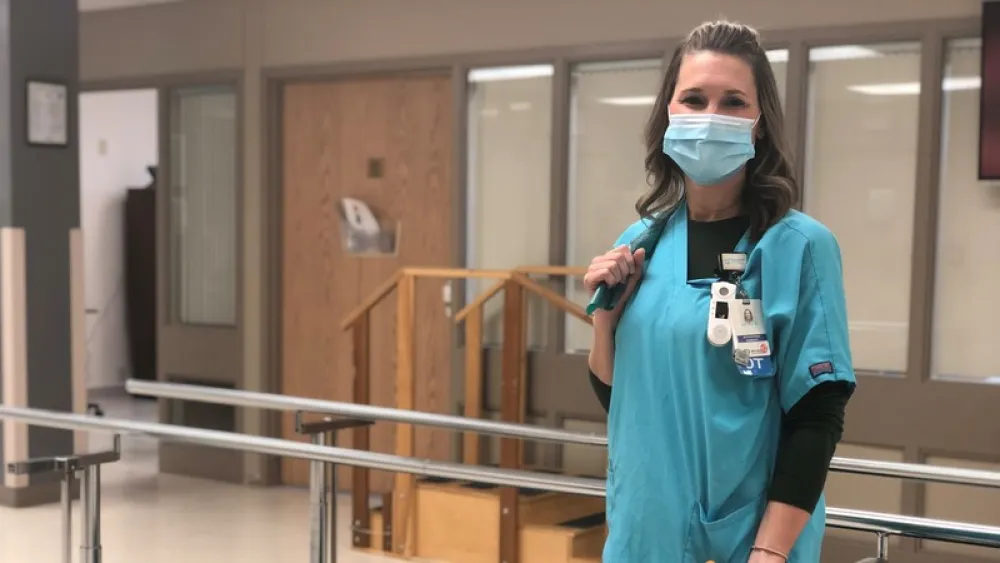
“Nobody really knows what we do,” said Holly Whitney, OTL/R, an occupational therapist at Methodist Jennie Edmundson Hospital. “People seem to know about physical therapists. They know about speech therapists. But we’re often referred to as the other therapists.”
“When we meet patients in the hospital, they’re usually very confused by our title,” said Alli Greene, OTL/R, CLT-LANA, an occupational and lymphedema therapist at Methodist Fremont Health. “They’ll say, ‘Occupation? I don’t need a job.’ Or, ‘I’m good. I haven’t had a job in years.’”
“Yeah, fortunately, we don’t give people career counseling in the hospital,” joked KC Humphrey, OTL/R, an occupational therapist at Methodist Hospital. “But we can help you do the jobs you need to do on a daily basis. And for some people, that job is simply to get on and off the toilet.”
But helping patients regain their normal function and necessary skills only skims the surface of what occupational therapists (OTs) do. That’s been especially true over the past year, as the COVID-19 pandemic has presented many of them with countless patients who’ve required so much more than just the strength and independence to complete their daily tasks.
Getting to Work
Early on in the pandemic, when Methodist was working diligently to limit the number of staff entering and exiting COVID-positive rooms, OTs were unsure whether they’d have much contact with COVID-positive patients at all.
“But about a month and a half in, the tides were turning, and it became clear that these patients needed us,” Greene said.
Like many COVID-19 warriors, Greene, Whitney and Humphrey had little fear about stepping up to the front lines.
“I was actually kind of excited because the complexity of these patients is something we don’t often see,” Greene said. “I mean, these patients had such horrible deficits. They couldn’t raise their arms. They couldn’t feed themselves. One couldn’t even hold a cellphone.”
So, with baby steps, they got to work.
“Maybe the first day it was going over how to brush their teeth in bed – or brushing their hair in bed,” Humphrey said. “Then, maybe we move to some activity while they’re sitting up on the edge of the bed. We kept pushing them gradually until we reached the point of, ‘OK, let’s get up and walk over to the chair now.’ And, ‘Great, now that you can handle that, let’s move over to the sink to brush your teeth.’”
Whitney added: “Even though it was all the things we were used to doing on a day-to-day basis, it was such a huge learning curve – knowing how hard to push and when to back off with these patients who’ve been ventilated or on so much oxygen for such a long time. And then just constantly reassessing their status to make sure you’re keeping them safe.”
Addressing Physical, Cognitive and Emotional Needs
It wasn’t only the physical care of these patients that challenged Methodist OTs. Many of them were forced to get creative in addressing each patient’s cognitive needs, too.
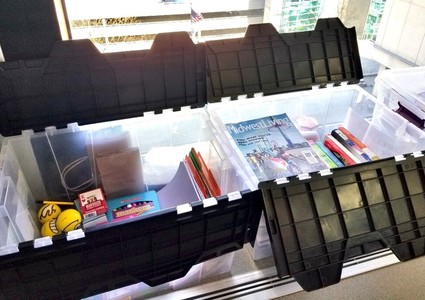
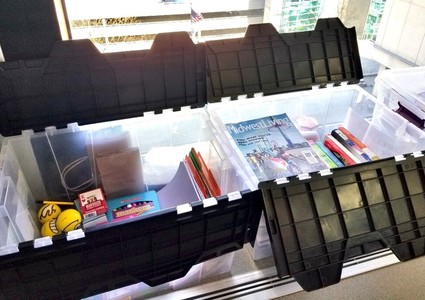
Humphrey and her colleagues took it upon themselves to organize "activity tubs" for patients dealing with brain fog – a common lingering symptom of COVID-19. Staff members were quick to support the cause, donating word searches, crossword puzzles, cards, phone chargers, reading glasses, adult coloring books, colored pencils and more.
“If you don’t use it, you lose it,” Humphrey said. “And getting these patients engaged in something – anything – actually proved to be very therapeutic. Otherwise, think about it – they’re just lying there, doing nothing. Some of them aren’t even watching TV.”
The activity tubs and other ideas, Humphrey said, came as part of her team’s holistic approach to care – which addresses a patient’s physical, cognitive and emotional well-being. And finding ways to address that last facet has proven to be the most gratifying of all, she added.
“I can’t tell you how many patients I hugged in all that PPE (personal protective equipment),” Humphrey said. “I can’t tell you how many times I took my cell phone, stashed it under my gown and played music for patients after finding out what kind they liked. Or how many times I sat and just listened to patients. Not necessarily, ‘Tell me what you’re going through.’ But, ‘Tell me about yourself, where you grew up, what you did for a living.’ Just being someone they could talk to face-to-face. During a time with no visitors, it was so wonderful to be able to love on people in that way.”
Whitney thinks often about the many patients she helped who had come from nursing homes.
“These patients hadn’t had visitors in weeks,” she said. “I had a lady tell me that she was so happy she got pneumonia so she could come in and actually see people. That’s heartbreaking – hearing patients say, ‘I’m tired of not being able to see my family. I don’t want to wave through a window anymore. I can’t hear on these iPads.’ But it was also pretty special to see how appreciated that in-person human connection was.”
Letting the Good Outweigh the Bad
That face-to-face connection is something Methodist OTs have deeply valued, too. Because over the past year, they’ve experienced their fair share of “I-can’t-believe-this-is-real-life moments,” as Whitney called them.
“Unfortunately, all the days I rushed into work early to check how many of my patients were still alive will probably always be a forever memory for me,” Greene said.
“As therapists, we tend to see people when they’re recovered,” Humphrey said. “It was very hard to look in the obituaries every day and see multiple patients of yours.”
But according to Humphrey, Greene and Whitney, the bittersweet goodbyes with patients who beat COVID-19 and regained the independence and peace of mind to live their lives again outweighs all the darkness that’s come out of this pandemic.
“And the teamwork,” Greene added. “It was just such a huge team effort, and I think that will live on forever here. The way we took care of those patients as efficiently as we did. It’s a pretty amazing thing.”
And it may be proof that it doesn’t take a well-known profession to make a really big difference.
“Helping people help themselves,” Whitney said. “That’s why I love what I do. Everyone always asks the question, ‘If you could do one thing, what would it be?’ It’s this. And it always will be.”
More Resources
- Learn more about occupational therapy at Methodist.
- Read about another group of unsung heroes: members of Methodist’s Incident Command System.
- Read more inspiring stories of Methodist patients and staff.


